May 15, 2014
More Illinois residents than originally projected are signing up for Medicaid as a result of the federal Affordable Care Act, but the long-term impact on the State budget remains unclear.
Illinois officials had initially projected that 241,500 new recipients would sign up by the end of the current fiscal year on June 30, 2014. The current enrollment estimate for year-end FY2014 is 78.1% higher at 430,000.
Medicaid is a joint federal-state program that pays for healthcare for certain categories of low-income people, including children, pregnant women, the disabled and the elderly. Medicaid expansion was one of the key provisions of the Affordable Care Act (ACA) designed to reduce the number of people without health insurance. Beginning on January 1, 2014, the ACA extended Medicaid coverage to nearly all adults with incomes up to 138% of the federal poverty level. In 2014 this means that a single person can have income up to $16,105.
The U.S. Supreme Court ruled in June 2012 that participation in the ACA Medicaid expansion was optional for states, and Illinois enacted a law authorizing the expansion in July 2013. Cook County’s public health system got approval from the federal government in October 2012 to begin signing up newly eligible Cook County recipients in Medicaid before the official start of the expansion in January 2014.
New Medicaid recipients under the ACA fall into two categories: individuals who are newly eligible under the law and those who were previously eligible but had not enrolled in the program. Previously eligible individuals were expected to enroll because of publicity surrounding the ACA and policies that steer individuals to Medicaid if they are not eligible to obtain insurance coverage through the new ACA-mandated health insurance exchange.
The Illinois Department of Healthcare and Family Services (HFS), the State’s main Medicaid agency, had projected that 161,000 of the 241,500 new enrollees at the end of FY2014 would be newly eligible under the ACA. The rest of the new recipients, approximately 80,500, were expected to be previously eligible but not enrolled. By the end of calendar year 2017, HFS projected a total of 509,000 ACA-related enrollees: 342,000 newly eligible individuals and 167,000 previously eligible but not enrolled recipients.
The following table compares original enrollment projections with current projections for the end of FY2014. HFS has not revised its enrollment estimates for 2017.
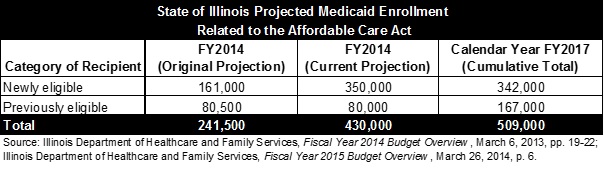
As shown in the table, estimated enrollment of previously eligible recipients has remained virtually unchanged. Newly eligible individuals have signed up much more quickly than expected, however. The projected total of 350,000 newly eligible enrollees at the end of FY2014 exceeds the estimate of 342,000 by the end of calendar year 2017.
In recent testimony to the General Assembly, HFS Director Julie Hamos said that the original projections did not fully take into account enrollment in the Cook County program. The program, known as CountyCare, is expected to account for more than 94,000 of the newly eligible enrollees—nearly 30%—at the end of FY2014.
Another 36,000 newly eligible recipients were enrolled based on participation in the Supplemental Nutrition Assistance Program (food stamps). Illinois is one of five states that got federal permission to skip most of the Medicaid application process for food stamp recipients.
The enrollment numbers for FY2014 are still in flux because the Illinois Department of Human Services, which handles Medicaid applications, has a large backlog of applications forwarded to the State from the federal online insurance exchange. It is not clear how many of those applicants will be found to be eligible for Medicaid.
HFS expects only a modest increase in ACA-related enrollment in FY2015. The total number of new ACA-related recipients is expected to increase by 40,000 to 470,000, including 35,000 newly eligible participants and 5,000 previously eligible individuals.
The federal government is scheduled to pay 100% of the cost for newly eligible recipients through 2016; 95% in 2017; 94% in 2018; 93% in 2019; and 90% thereafter. Medicaid spending for previously eligible individuals who enroll because of the ACA will be reimbursed by the federal government at the regular rate—50.76% for Illinois in FY2015—rather than at the ACA expansion rate. The State share of Medicaid costs for Cook County residents is covered by the County rather than by the State.
The cost of the Medicaid expansion depends on both the number of new recipients and their average use of Medicaid services, which is tied to the medical condition of new enrollees.
After Governor Pat Quinn presented his FY2014 budget proposal in March 2013, HFS increased its estimate of average medical expenses for each category of ACA enrollee by approximately 66%. These estimates, which were reflected in the enacted FY2014 budget, have not been revised.
It is too early to reassess average spending for new recipients, according to State officials, because of delays in the receipt of medical claims and the tendency to use services more intensively over time.